
Radiotherapy is one of the treatments that can be given to people with breast cancer and in this article two therapeutic radiographers from Rad Chat provide insight into what to expect together with tips to help make radiotherapy treatment as comfortable as possible for you.
By Jo McNamara and Naman Julka-Anderson
References to numbers in brackets throughout the text refer to the references at the foot of the article.
Before radiotherapy: start making healthy lifestyle choices as soon as you can.
This will enable you to be in the best possible shape ready for your treatment.
- If you smoke, seek support for smoking cessation ASAP. Your radiotherapy side effects (such as skin reactions) are likely to be more severe if you smoke through treatment (1,2).
- Start to omit alcohol where you can as it dehydrates you and can increase symptoms of fatigue (2). There is support available for patients who depend on alcohol and need help to quit drinking, this will in turn improve your overall health, as well as lessen your side effects.
- Radiotherapy does cause a lot of cellular damage and so increasing your fluid intake will help with repair and growth. We suggest between 2 litres of fluid a day, so also try to ditch the tea and coffee which are diuretics and will make you urinate more and can actually dehydrate you, switch to the water instead. Maintaining hydration can also help with the symptoms of fatigue
- Start to make positive changes to your diet, lots of fruit and vegetables, fibre and protein. This will help with cellular repair and also assist with fatigue (3).
- Engage in physical activity, walk to the local shop, rather than drive, go for a walk rather than watching the TV. Being out in fresh air and getting some exercise is beneficial for your physical and mental health and can also boost your energy (4). It’s important to only engage in physical activity that suits your capabilities.
Helpful resources are:
- Get help for Smoking cessation www.nhs.uk/live-well/quit-smoking/nhs-stop-smoking-services-help-you-quit/
- Local smoking cessation www.nhs.uk/better-health/quit-smoking/find-your-local-stop-smoking-service/
- Alcohol Support www.nhs.uk/live-well/alcohol-support/
- Increasing your physical activity with peer support: www.5kyourway.org
Mental health support is available
It’s important to acknowledge what you’re going through is difficult, both emotionally and physically. Your oncology team will help you find a new normal. Radiotherapy, even when being used to cure your cancer, can leave you with lasting consequences. This will vary between people but be aware that radiation can cause late effects further down the line. Late effects can arise from 6 months to 20+ years post-treatment. Starting to process this and adapt physically to your new body can be challenging and be open to accessing support and advice for your mental well-being.
Helpful resources are:
- Mind Charity www.mind.org.uk/
- NHS Talking Therapies www.nhs.uk/mental-health/talking-therapies-medicine-treatments/talking-therapies-and-counselling/nhs-talking-therapies/
- Mindfulness www.nhs.uk/mental-health/self-help/tips-and-support/mindfulness/
Know that your mobility might change
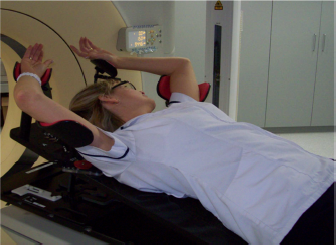
After having surgery it is often the case that arm mobility is affected. In radiotherapy we need patients who are having breast or chest wall radiotherapy to raise their arms above their heads for several minutes a day. Make sure you follow the physiotherapy exercises recommended by your team religiously after surgery to ensure you can comfortably complete your radiotherapy course. Also consider doing simple exercises around the house to improve your mobility, for example reaching to put cans on a high shelf. This will also help you maintain your mobility after you’ve finished your treatment (5).
Some mobility exercises to do post surgery:
- Breast Cancer Now www.breastcancernow.org/sites/default/files/publications/pdf/bcc6_exercises_booklet_2019_web.pdf
- Get me Back PT trainer www.getmeback.uk/
Radiotherapy techniques
For some patients having radiotherapy to their left side, you may be asked to do a specific breathing technique to help minimise the dose to your heart (6). This can be a tricky technique to master so there are resources available to help prepare you prior to treatment, for example, Respire www.respire.org.uk/resources.
To align you every day in the correct position, you may be asked to have permanent tattoos. These are tiny pin prick tattoos, typically placed on the left and right side of your rib cage and one centrally. These are used to ensure you are set up in exactly the right position each day for accurate, reproducible treatment. There is a new emerging technique called surface guided radiotherapy, which uses cameras to match the contour of your body to help get you into the correct position everyday (7).

What to bring to a radiotherapy appointment
If you are working, have caring responsibilities, or know that you struggle to get going in the mornings then do ask the therapeutic radiographers for appointments to suit your circumstances. We cannot always accommodate your requests, but we will try! The radiotherapy treatment itself is fairly quick and can take as little as 5 minutes and as long as 25 minutes.
- If you feel anxious during the treatment, why not consider bringing some music to play.
- Occasionally there may be delays for treatment, or if you are waiting for a specialist for a treatment review, so we advise that you bring something to take your mind off waiting, such as a book, phone/tablet or crochet/knitting pattern.
- You may also want to bring a drink, some snacks and any medical information you may need e.g. list of medications or questions you want to ask.
- It can also be helpful to record your conversations with your oncologist or therapeutic radiographers if you know you struggle to retain information.
- It can sometimes feel overwhelming with the amount of information you are given but please don’t hesitate to ask staff to clarify anything you are unsure of or forgotten!
- Many radiotherapy departments will have a designated website and many provide information about what to expect, so please do go on and have a look.

Ask to look at your radiotherapy treatment plan
Although you may not be able to interpret your radiotherapy treatment plan, asking your therapeutic radiographer to go through it with you will show you where the radiation is actually targeting and will highlight where you will get the effects of radiation. Every radiotherapy treatment plan is personalised to you and that is one of the reasons why everyone’s experience of radiotherapy side effects is different.

Skincare during radiotherapy
Many patients will experience a radiotherapy skin reaction. This is not a burn, although it can have characteristics which are similar. Looking after your skin prior to, during and after radiotherapy will help. Severe skin reactions aren’t normally seen due to advancements in radiotherapy treatment techniques. If you do notice a skin reaction, this will only be seen within the area you are being treated (8).
For patients with lighter skin tones, you might notice your skin within the treatment field may become pinker or redder. For patients with darker skin you may notice some faint redness, or that the treatment area looks darker or more pigmented. Speak to the treatment therapeutic radiographers or the treatment review team if you have any concerns or need some advice. Even when you have finished radiotherapy you may go on to experience skin reactions, which is totally normal, please do contact your radiotherapy team if you need advice and support.
This is the latest evidence based skin care guidance created by the Society College of Radiographers.
Managing fatigue from radiotherapy
Radiotherapy causes fatigue. This is not just feeling tired and it may surprise you that doing physical activity will actually help manage fatigue(9). Personalise the activity for you. It doesn’t have to be a gym session, it could be 30 minutes of hoovering. It doesn’t have to be a run, it could be a gentle stroll. You know your body better than anyone else, so use that knowledge to pick the activity appropriate for you but try to keep active and get out of the house into nature if you can.
Helpful resources are:
- Increasing your physical activity with peer support www.5kyourway.org/
- Managing fatigue www.macmillan.org.uk/cancer-information-and-support/stories-and-media/booklets/coping-with-fatigue-tiredness
- Sleep and mental health www.mind.org.uk/media-a/5827/sleep-problems-2020.pdf
- Fatigue www.breastcancer.org/treatment-side-effects/fatigue
Understanding your body
Your body will go through a lot during your cancer treatment. It’s okay to feel differently about your body after this. It’s okay to be reluctant to consider being intimate with a partner. It’s about finding your new normal, finding your comfort zone and loving your body how it is.
If you’re struggling with body confidence there are many feel good workshops you can access through your local department. You can also speak to your local Boots about working with a Boots Macmillan Beauty Advisor.
Sex and intimacy can be important to people in different ways. It’s about taking things slowly and ensuring you are ready for this post treatment. Sometimes a conversation with our partner is all you need or you can access a psychosexual specialist through your department for professional support. For example, check out, www.jodivine.com/blogs/sexual-health/sex-and-breast-cancer
Self-examination after breast cancer is very important as this will help you be more self-aware of your body and ensure you know how to feel for any further. Look at these links:
- www.coppafeel.org/info-resources/health-information/#howdo
- www.nhs.uk/common-health-questions/womens-health/how-should-i-check-my-breasts/
Use your Therapeutic Radiographers to support you through treatment
It can be easy to be a passive patient and just follow instructions blindly without asking why or getting more information if you require it. Ask the therapeutic radiographers all the questions. We are experts in radiotherapy and so if you aren’t sure of what to do, or why, please do ask!
Every patient is different, and you may not wish to know what is happening, or you may wish to know everything, we will be governed by you. We are here to support you through your radiotherapy treatment and beyond.
Within your radiotherapy department you will meet a wide range of therapeutic radiographers: for your initial appointment you might meet a consultant therapeutic radiographer who may consent you for treatment, a pre-treatment therapeutic radiographer who will help take your CT (planning) scan and may give you permanent tattoos if you need them. A dosimetrist or medical physicist will design your personalised radiotherapy treatment plan, and a treatment therapeutic radiographer who will deliver your treatment and answer any questions you have. You may also have a treatment review therapeutic radiographer who will be checking in on you during and after your radiotherapy. If you don’t know who someone is, or what their role within your treatment pathway is, please ask them!
Gain information from the right sources
It is fantastic to see so many cancer patient resources available now, as well as patient advocates sharing their experiences on social media and on blog pages. Please be aware everyone’s experience of cancer and treatment is personal to them and so accessing information is important from a reliable evidence-based source. Always look at people’s qualifications, consider the medical evidence supporting the advice and stick to UK based information, as cancer treatment and specifically radiation treatments vary significantly across the globe.
Our go to resources are:
- www.rcr.ac.uk/guidelines
- www.macmillan.org.uk/
- www.breastcancernow.org/
- www.nhs.uk/conditions/breast-cancer/
- www.radchat.transistor.fm/
Dose and Fractionation
Please try not to compare your radiotherapy regime to others. Your oncologist, or consultant therapeutic radiographer will prescribe the best radiotherapy dose and fractionation for you. Some patients may just receive 5 treatments and others may receive many more, this is dependent on lots of factors and the department’s radiotherapy protocol. Please ask for clarification when being consented for radiotherapy (10) .
References:
- https://bjui-journals.onlinelibrary.wiley.com/doi/10.1111/bju.12969
- https://www.sciencedirect.com/science/article/abs/pii/S1877782118302388?via%3Dihub
- https://be.macmillan.org.uk/Downloads/beMacmillan%20PDFs/MAC13612_Healthyeating_E03_LOWRES_20200206_KA.pdf
- https://www.macmillan.org.uk/documents/aboutus/health_professionals/physicalactivityevidencebasedguidance.pdf
- https://www.bmj.com/content/375/bmj-2021-066542
- https://www.rcr.ac.uk/sites/default/files/breast-cancer-treatment-covid19.pdf
- On target 2: updated guidance for image-guided radiotherapy | The Royal College of Radiologists (rcr.ac.uk)
- https://www.sor.org/getmedia/6cc80174-4478-4cd2-b501-35b41aae820d/2020_version_4_final_practice_guideline_radiotherapy_skin_care_llv1.pdf_2#:~:text=Radiation%20may%20cause%20chronic%20late,the%20scope%20of%20this%20document.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5891725/
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30932-6/fulltext
About the author
Jo McNamara and Naman Julka-Anderson are the hosts of Rad Chat – an oncology focused podcast for both patients and professionals. They are both Therapeutic Radiographers; Jo is an academic involved in the training and education of healthcare professionals in oncology, and Naman works as a Macmillan Treatment Review Radiographer in the NHS. Together they have compiled their top tips for breast cancer patients having radiotherapy using their combined 25 years’ worth of experience. Rad Chat always advises patients to talk to their oncologist and therapeutic radiographers about their individual radiotherapy treatment.
Further information
Future Dreams hold a range of support groups, classes, workshops and events to help you and your carers during your breast cancer diagnosis. These are held both online and in person at the London-based Future Dreams House. To see what’s on offer and to book your place, see here.
To return to the homepage of our Information Hub, click here where you can access helpful information, practical advice, personal stories and more.
Reviewed February 2023
Next review date February 2026
The information and content provided in all guest articles is intended for information and educational purposes only and is not intended to substitute for professional medical advice. It is important that all personalised care decisions should be made by your medical team. Please contact your medical team for advice on anything covered in this article and/or in relation to your personal situation. Please note that unless otherwise stated, Future Dreams has no affiliation to the guest author of this article and he/she/they have not been paid to write this article. There may be alternative options/products/information available which we encourage you to research when making decisions about treatment and support. The content of this article was created by Jo McNamara and Naman Julka-Anderson and we accept no responsibility for the accuracy or otherwise of the contents of this article. The links and/or recommendations in this article to third-party resources are for your information and we take no responsibility for the content contained in those third-party resources. Any product recommendations made in this article are not product endorsements and unless otherwise stated, they are made without any affiliation to the brand of that product. We ask you to note that there may be other similar products available.
Share

Support awareness research
Donate to those touched by BREAST cancer
Sylvie and Danielle began Future Dreams with just £100 in 2008. They believed nobody should face breast cancer alone. Their legacy lives on in Future Dreams House. We couldn’t continue to fund support services for those touched by breast cancer, raise awareness of breast cancer and promote early diagnosis and advance research into secondary breast cancer without your help. Please consider partnering with us or making a donation.


