
TRIGGER WARNING: THIS ARTICLE DISCUSSES SECONDARY BREAST CANCER
In this Q&A Jo talks about the works she’s doing to help raise awareness of secondary breast cancer, push for new treatments and provide support for those living with the disease. And she’s doing all of this whilst living with secondary breast cancer herself.
By Jo Taylor
- Can you start off by telling us a little bit of background on your breast cancer diagnosis and treatment ?
I’m Jo Taylor – I had primary HER2+ BC back in 2007 at age 38 whilst on maternity leave with my then 5 month old daughter and 2.5 year old son. I had no close family member who had breast cancer or I believe any paternal relative that had it. I live in a beautiful area in Manchester called Saddleworth and had moved here just 8 months previously. I was in bed one morning as my husband had gone downstairs, lifted my right arm and scratched underneath the area with my left hand and felt a small lump. The size of my little finger nail. I didn’t tell my husband and worried all that Sunday and the Monday made an urgent appointment at the GP and I was on the conveyor belt of a 2 week wait pathway with mammogram, biopsy and then being told 2 weeks later I had “a small breast cancer”. Shocked. It was “belt and braces” time with a full mastectomy with immediate Latissimus dorsi breast reconstruction, 6 chemo, 3FEC and 3 taxol (allergic to taxol so ended up with 5 FEC) then 20 radiotherapy sessions and was put on tamoxifen for 5 years. I was told they would keep me for five years in follow-up.
2. You were diagnosed with secondary breast cancer some time after you’d initially been treated for primary breast cancer. At the end of your primary breast cancer treatment were you told about the risks of secondary breast cancer and what to keep a look out for?
I was diagnosed 7 years after my initial primary breast cancer. I have never formally been told about any red flag symptoms of SBC but when I would go for appointments every 6 months (alternative one with a surgeon and the next with an oncologist) they would always check my breast area and under the axilla (armpit) and neck for any lumps. I had a recurrent chest infection which I had an xray for and was told at the time probably not helped with what looked like scaring on the lung due to radiotherapy treatment I had for the original primary BC. But there were no concerns with the lung scaring. Everything was OK and yearly mammograms would come around with “no worries or concerns reported”. I had also seen a report at SABCS – San Antonio Breast Cancer Symposium – that it was beneficial to have tamoxifen for 10 years instead of 5 years and I rang my oncologist immediately and scheduled a chat with her about this. She wondered how I had this information but as an informed patient I had the connections and knowledge to ask about this. I was adamant that it would be beneficial and it scared me that I wouldn’t be on tamoxifen when I was only 38 diagnosed and felt this would at least give me another 5 years without having to worry more about SBC if I wasn’t on any oestrogen blocker. The side effects outweighed the risk for me and I would deal with tamoxifen SEs as long as it protected me against getting secondary breast cancer.
3. What led you to set up your website www.abcdiagnosis.co.uk and can you tell us a bit about the site?
I had launched my website www.abcdiagnosis.co.uk on my 6th “Cancerversary” which is a one stop shop with information, peer support, signposting as well as choices for reconstruction as I had a poor experience with my own reconstruction and ended up having surgery at a different hospital. That was the main reason “patient choice” for the website. I hated that not all women would seek out a second opinion or go ask for another consultation with another surgeon. I wanted to empower women to be able to do this. Your body is important and these are life changing decisions which shouldn’t be made with a couple of photos or no photos at all. Research and information was important and crucial and it’s a time that you have to make quick decisions when information isn’t at your fingertips. Many didn’t know which sites or support to have and I wanted to share what I had gathered to support women. The decision to start it was back at a photo shoot for Red Magazine about myself and 3 other women friends who had supported each other through our breast cancer diagnosis. I’m still in touch with Jo and Mandy, sadly Debbie died a year later. This was my first experience of someone dying of secondary breast cancer and the devastation of a young family (2 twin girls who were around age 4). It was a very hard time.
4. A couple of years ago I attended one of your abcdiagnosis retreats and it was such a huge help for me in picking up exercise after treatment and moving forward. Can you tell us a bit about these retreats?
I had jogged prior to breast cancer and it took me a year after my diagnosis to get my running shoes back on and be able to do this. I wish I had continued to exercise all the way through my primary treatment. But clinical staff tell you you will be tired and worn out and just sit and do nothing. It’s the wrong thing. I put on weight and felt depressed. I started running again and everything went well with a 10k at 61 mins which I was gutted about as wanted to break the hour (I know that to you runners out there that time is probably pathetic but hey I’d had breast cancer!). I knew that exercise didn’t just help me physically but mentally too. I felt motivated running and would run and chat with friends when we run together. I knew when I was diagnosed with SBC that I would continue to exercise in fact I upped my exercise with running, cycling, walking, yoga and even cross fit. I’m a passionate advocate for exercise through, after and living beyond a cancer diagnosis.
I wanted other BC patients to experience the motivation and the enjoyment of exercise. Exercise shouldn’t be a chore and you need to fit it into a normal day and it become a habit. I held the retreat a 2 night 3 day retreat (currently on hold due to COVID) in Saddleworth where I live and this was for motivational exercise for patients. It is short bursts of an hour of jogging, cycling, yoga and Nordic walking and in-between some holistic therapies as well as down time with new friends. I realized that the peer support that this was creating, was a huge part of the retreats, and many of the groups still chat to each other. The support and motivation it gives others is huge. And I was there to show that I could do all this exercise too. As a SBC patient, I was really breaking down barriers about the disease, talking openly as well as showing that exercise can be fun and we all just need a little help to get started. The idea is that the motivation is taken home and you get others to support you and maybe go out with you also to do exercise – using friends and family as exercise buddies an in turn actually it can help them too. Any movement is great for anyone. The retreats have gone from strength to strength. I’ve had participants from England, Ireland, Scotland and Wales. People from the USA and further afield have said they want to attend. There isn’t much like this out there that has a cancer patient leading a retreat or this idea. I feel that is the USP.
5. One the most helpful things about your site are the SBC red flag infographics – what led you to create these?
I created the red flag infographics due to a SBC conference I attended at my hospital where my CNS mentioned red flags to all attendees, and at the end I approached her and asked her “why are you not sharing this information with primary patients?” The response was that it was “too scary”. And my Oncologist agreed?! And then I found out that charities agreed… And as a patient I KNEW that this was wrong so decided to create an infographic to show visually where breast cancer can metastasize to, as well as the red flag signs to look out for. A simple 1 page document. It was developed over 5/6 years to what we have now but after attending a NHSEngland conference to talk about the infographics, they decided to signpost to the infographics and have advised all Cancer Alliances across England to share this information and filter it down to their hospitals. The idea is that the infographics are provided at the end of primary treatment in a PCP – Personalized Care Plan – this document is there for reference about all issues you may have and your treatment e.g. a holistic needs assessment. Then if you need bisphosphonates or fertility support or whatever it may be, it’s a written document. Basically a record so you don’t forget to ask all the relevant questions. The infographics will be in there and this will open up a discussion about risk and red flag symptoms to look out for – possibly around a year after you have finished surgery and treatment (like chemo and radiotherapy).
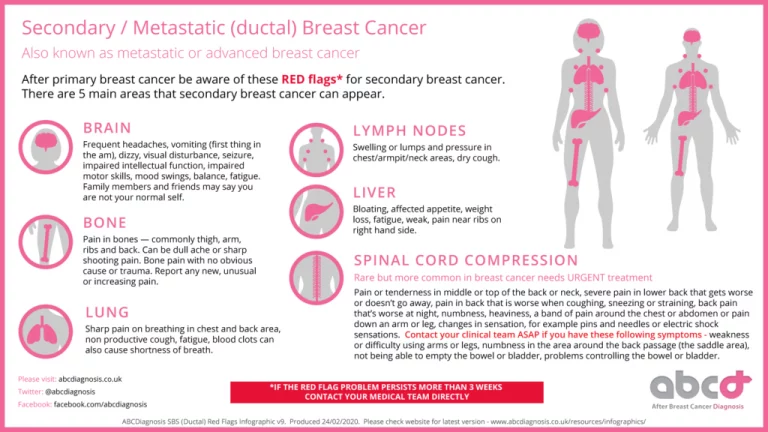
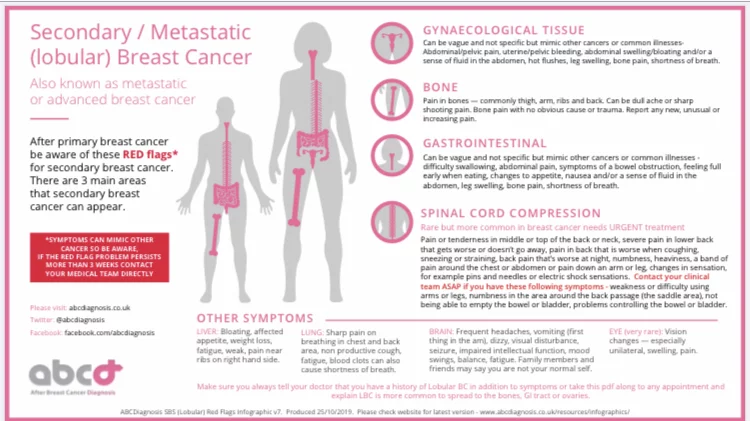
Currently it is being included in The Christie PCP document for breast cancer patients – so being ratified and signed off. So many times I’ve heard patients have missed red flag symptoms and their GP has not linked them with breast cancer. The joined up care doesn’t seem to happen. This is wrong and it needed to change so that’s why I developed it. I’ve had patients contact me to say they have taken the infographic with them to appointments and sadly they are re-diagnosed but are thankful that they had this document to make sure that they didn’t get fobbed off by a GP or clinical person. Now Gateway C (a GP portal) have this information too, and hopefully GPs will learn about this or at least use it as a referral document. With any “open access” breast cancer clinics it is also very important that this information is available as you are relying on patients to recognise these symptoms. If you don’t empower them with this information then you are failing your patients.
Around 30% of early stage breast cancer patients will “at some point” (and for some disease types that can be 20 years later) metastatise and develop SBC. Patients need early diagnosis and early treatment as survival for them can be better if they get the right treatment asap. Surely its better to have a couple of small areas of disease that can be treated, rather than leaving it and having multiple sites that are too hard to treat with surgery, radiotherapy or chemo? It’s a no brainer for me. Some patients also are diagnosed with what is called DeNovo SBC which means that no primary was detected and they presented with SBC red flag symptoms. This is why it is important for AWARENESS to not just be about primary disease. Patients don’t always find a lump and can have symptoms of SBC at the same time. And remember there are other breast cancer types like inflammatory breast cancer or Pagets BC that don’t even present with a lump!
6. Can yell us a bit about www.metupuk.org and your involvement in this group?
A few days before my 7th Cancerversary I was rediagnosed with incurable secondary breast cancer. After being diagnosed I started more advocacy, campaigning and activism due to the many issues in the UK with drug access, clinical trials as well as no mandatory data and statistics collected for secondary breast cancer. I connected with Beth Caldwell who founded METUP in the USA and a year or so later asked if I could create a UK arm of METUP so formed METUPUK. The movement has been growing and we now have a website. We have aims and objectives, and we campaign to make change which will help patients to live longer. We aim for the disease to be changed from a terminal/incurable disease with a 2-3 year median life expectancy to a chronic disease where people are living 10/15/20 years after diagnosis. This is based on what happened with HIV and ACTUP – our organization is founded on their activism, upset and anger at a system that is failing them and change is needed.
7. In addition to your own website and your work on metupuk.org, you work hard as a patient advocate on behalf of secondary breast cancer patients – what sort of things does this involve?
I am involved in the Greater Manchester Breast Pathway Board as a patient representative. I attend the steering groups for the ECMC – Experimental Cancer Medicine Centre – which is for early phase trials before patients are involved. I regularly share my personal story with clinical personnel as well at attending conferences in the UK and Europe like ESMO – European Society of Medical Ongology. There is always lots going on in breast cancer whether clinical research or trials or with other organizations and I search them out and attend or nowadays have a zoom meeting. I find it important to stay informed and up to date with everything that is going on which is why I like Twitter as it is a huge platform for gathering information and sharing information and connecting with some amazing people, patients as well as clinicians, researchers etc. Recently I attended a zoom which led me to question why DIBH – deep inhalation breath hold technique – wasn’t being used at The Christie and then after I tweeted it wasn’t being used across the UK – so I contacted Action Radiotherapy and spoke to Kim Meeking and Prof Pat Price (who was recently on Panorama) who first of all were shocked at the inequalities after seeing my thread and secondly agreed and put a plan into place to address this. Its currently being reviewed and they are hopeful that all hospitals WILL follow the NICE guidelines that are in place but not being followed!
8. How could someone get involved in patient advocacy?
Join a group, listen, learn and get involved. No one will think you are silly or stupid – it’s all about learning, having empathy and understanding and sharing the good work. I knew very little before breast cancer and every day I learn something different and I pass this knowledge on. I love learning, helping and I’m committed to making change. And this isn’t just about SBC patients as you see from the DIBH radiotherapy issue, this affects primary patients too. There are ALWAYS improvements to be made. If someone says there isn’t, that’s rubbish. And please don’t wait as a primary patient to get SBC before you are a patient advocate – we need ALL voices to join together as only patients can change problems. There are online groups or connect with abcd or metupuk and feel free to join us! We welcome everyone and you could even be a family member or a friend, it really doesn’t matter, it’s about sharing the messages and helping to make the necessary change. The more people we have the better to challenge and change these systems. The only way we can make change is by patients pushing these issues. One of my favourite quotes by Margaret Mead is “Never depend on any governments or institutions to solve any major problems. All social change comes from the passion of individuals.” I truly believe this is the case.
9. What is your advice for people who have completed treatment for primary breast cancer in terms of staying vigilant in respect of the signs of secondary breast cancer?
Do not leave any symptom for long. As previously said, it is better for your long term survival to address any issue. Don’t let anyone tell you its nothing if it’s a nagging problem. Trust your instinct. If you do not think you are getting the right support see someone else. You have to be your own advocate in many instances. You know your own body if its worrying you tell them. And don’t put it off. Like the current campaign in the media please #HelpUsHelpYou
10. Do you have some resource recommendations for people who have recently been diagnosed with secondary breast cancer?
Have a look on my website where I share many resources as a “one stop shop” – there is a huge amount of information out there but not necessarily the right information. ABCD and METUPUK provide lots and my book* also talks about evidenced based treatment as well which is very important when people who do not know or understand cancer share information about “alternative treatments”. As Dr Robert O’Connor advises “If its too good to be true, usually it is.” And join the breast cancer social media community whether on Twitter or Facebook – you will find your “tribe” and you will gain a great support group and many times end up additionally with some life long friendships.
*Jo’s book, is a free book for all primary and secondary breast cancer patients filled with personal stories and helpful information. You can order a free copy from Jo’s website here.
To return to the homepage of our Information Hub, click here where you can access more helpful information, practical advice, personal stories and more.
Future Dreams hold a range of support groups, classes, workshops and events to help you and your carers during your breast cancer diagnosis. These are held both online and in person at the London-based Future Dreams House. To see what’s on offer and to book your place, see here.
September 2020 (Reviewed February 2024)
This article was written by a guest author based on their own experience of breast cancer and its treatment. It is important to note that this is one person’s experience and that whilst there may be commonalities between the experiences of different people, everyone has a different diagnosis/treatment plan/general experience. The information and content provided in all guest articles is intended for information and educational purposes only and is not intended to substitute for professional medical advice. It is important that all personalised care decisions should be made by your medical team. Please contact your medical team for advice on anything covered in this article and/or in relation to your personal situation. Please note that unless otherwise stated, Future Dreams has no affiliation to the guest author of this article and he/she/they have not been paid to write this article. There may be alternative options/products/information available which we encourage you to research when making decisions about treatment and support.
Share

Support awareness research
Donate to those touched by BREAST cancer
Sylvie and Danielle began Future Dreams with just £100 in 2008. They believed nobody should face breast cancer alone. Their legacy lives on in Future Dreams House. We couldn’t continue to fund support services for those touched by breast cancer, raise awareness of breast cancer and promote early diagnosis and advance research into secondary breast cancer without your help. Please consider partnering with us or making a donation.



